

The patient must have FEV 1 below 40% of normal range. MELD 22 with 10% increase every 3 months as long as tumor is controlled by the treatment protocol and there is no evidence of metastases.Ĭystic fibrosis. The liver center requesting the MELD exception must have a written United Network for Organ Sharing–approved protocol that includes neoadjuvant chemoradiation and pretransplantation operative staging to exclude metastatic disease. These patients are listed with MELD 22 with 10% increase every 3 months if the Pa o 2 remains under 60 mm Hg.Ĭholangiocarcinoma. The patient must have evidence of intrapulmonary shunt and Pa o 2 below 60 mm Hg on room air. Other exceptions can include patients with the hepatorenal syndrome ( Chapter 144), the portopulmonary syndrome ( Chapter 144), cholangiocarcinoma ( Chapter 146), cystic fibrosis ( Chapters 83 and 137), familial amyloid polyneuropathy ( Chapter 179), and primary hyperoxaluria ( Chapter 194) ( E-Table 145-1). As a result, the MELD score is now adjusted for serum sodium concentration in allocating deceased donor livers (MELD-Na).
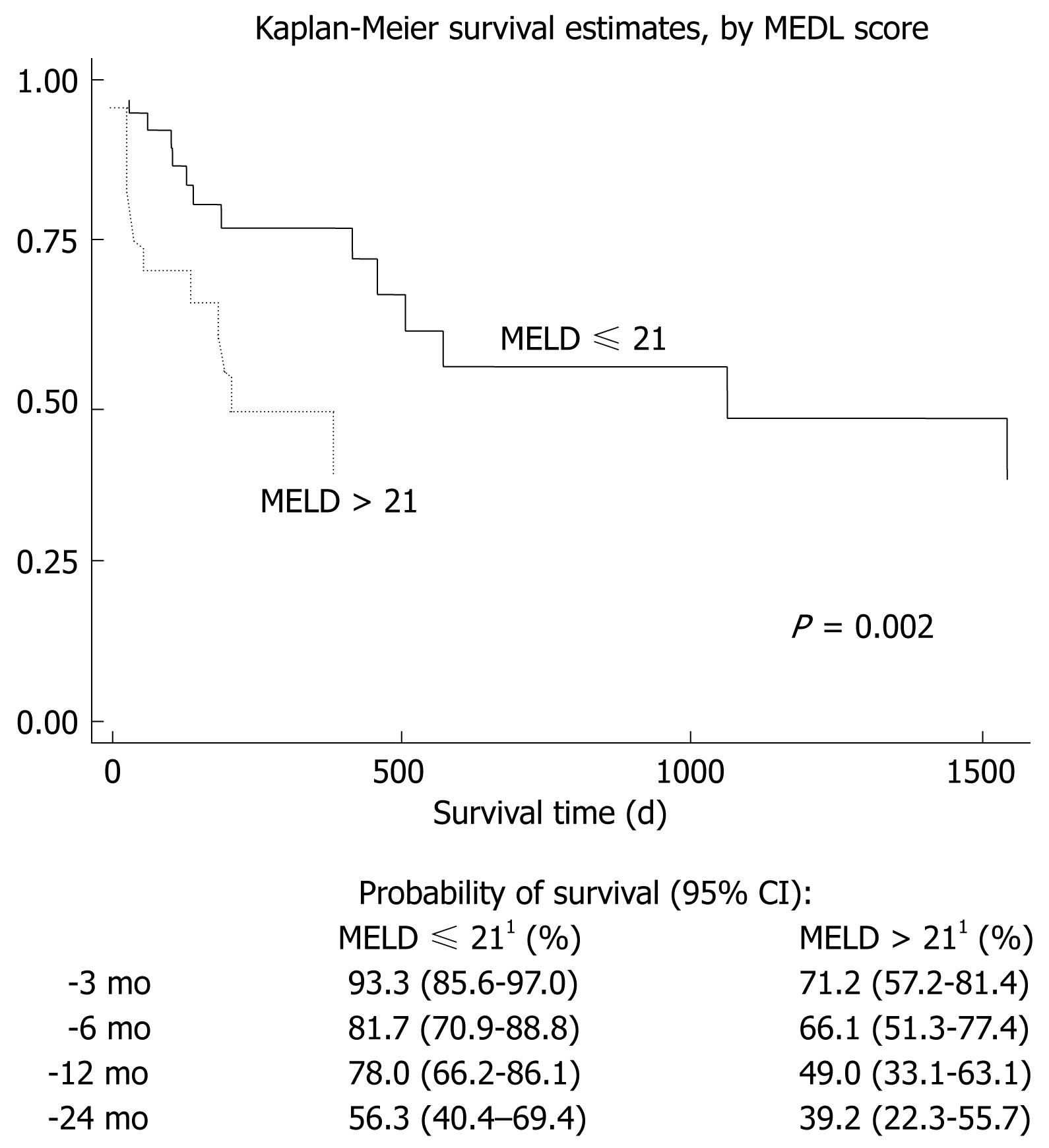
Hyponatremia is an independent predictor of mortality up to a MELD score of 30. In patients with cirrhosis ( Chapter 144), hyponatremia ( Chapter 108) is associated with hepatorenal syndrome, ascites, and death from liver disease. This allocation system has improved transplantation rates and has not altered waiting list or post-transplantation mortality. Patients with acute liver failure or post-transplantation patients with graft failure due to hepatic artery thrombosis have a MELD score of 40 and top priority status. In addition, the SHARE 35 rule allows for regional sharing of a donor liver to a regional patient with a score of 35 or higher. As a result, deceased donor livers must be made available more broadly if no local patient has a MELD score of 15 or higher. A patient’s survival is not improved by deceased donor liver transplantation if the MELD score is below about 15. The 3-month mortality rate increases from 10% with a MELD score of 20 to 60% at a MELD score of 35, and essentially to 100% with a MELD score above 40. liver transplantation candidates and the allocation of deceased donor livers are based on the MELD or MELD-Na score (see Table 144-2 in Chapter 144), which ranges from 6 (best prognosis) to 40 (worst prognosis). if bilirubin is 0.8, a value of 1.0 is used).Lee Goldman MD, in Goldman-Cecil Medicine, 2020 Assigning Priority: Model for End-Stage Liver Disease If the patient has been on dialysis twice in the past 7 days, the serum creatinine value used should be 4.0 mg dL -1 Īny value less than 1 is given the value 1 (i.e. All values above 40 receive a score of 40 The maximum score for the MELD score is 40. The following remarks to be made for this calculation are: It is calculated according to the following formula: This score is also used by the United Network for Organ Sharing (UNOS) and Eurotransplant to prioritize the distribution of liver transplants. It uses serum total bilirubin, serum creatinine, and INR values to predict survival. It was initially developed to predict the vital prognosis three months after surgery in patients who underwent an intrahepatic shunt via the transjugular route. The Model for End-Stage Liver Disease (MELD) score, or MELD Score or MSc, is a scoring system for assessing the severity of the chronic liver disease. Assessment of Hepatic Cirrhosis Severity Meld Score


 0 kommentar(er)
0 kommentar(er)
